Mycobacterium tuberculosis is a near-perfect predator. In 1882, Robert Koch, the physician who discovered the microbe, told a room full of scientists that it caused one in seven of all deaths. In 2023, after a brief hiatus, tuberculosis regained from COVID its status as the world’s deadliest infectious disease—a title it has held for most of what we know of human history.
Some people die of TB when their lungs collapse or fill with fluid. For others, scarring leaves so little healthy lung tissue that breathing becomes impossible. Or the infection spreads to the brain or the spinal column, or they suffer a sudden, uncontrollable hemorrhage. Lack of appetite and extreme abdominal pain can fuel weight loss so severe that it whittles away muscle and bone. This is why TB was widely known as “consumption” until the 20th century—it seemed to be a disease that consumed the very body, shrinking and shriveling it. On a trip to Sierra Leone in 2019, I met a boy named Henry Reider, whose mix of shyness and enthusiasm for connection reminded me of my own son. I thought he was perhaps 9 years old. His doctors later told me that he was in fact 17, his body stunted by a combination of malnutrition and tuberculosis.
The cure for TB—roughly half a year on antibiotics—has existed since the 1950s, and works for most patients. Yet, in the decades since, more than 100 million people have died of tuberculosis because the drugs are not widely available in many parts of the world. The most proximate cause of contemporary tuberculosis deaths is not M. tuberculosis, but Homo sapiens. Now, as the Trump administration decimates foreign-aid programs, the U.S. is both making survival less likely for people with TB and risking the disease becoming far more treatment-resistant. After decades of improvement, we could return to something more like the world before the cure.
Anyone can get tuberculosis—in fact, a quarter of all humans living now, including an estimated 13 million Americans, have been infected with the bacterium, which spreads through coughs, sneezes, and breaths. Most will only ever have a latent form of the infection, in which infection-fighting white blood cells envelop the bacteria so it cannot wreak havoc on the body. But in 5 to 10 percent of infections, the immune system can’t produce enough white blood cells to surround the invader. M. tuberculosis explodes outward, and active disease begins.
Certain triggers make the disease more likely to go from latent to active, including air pollution and an immune system weakened by malnutrition, stress, or diabetes. The disease spreads especially well along the trails that poverty has blazed for it: in crowded living and working conditions such as slums and poorly ventilated factories. Left untreated, most people who develop active TB will die of the disease.
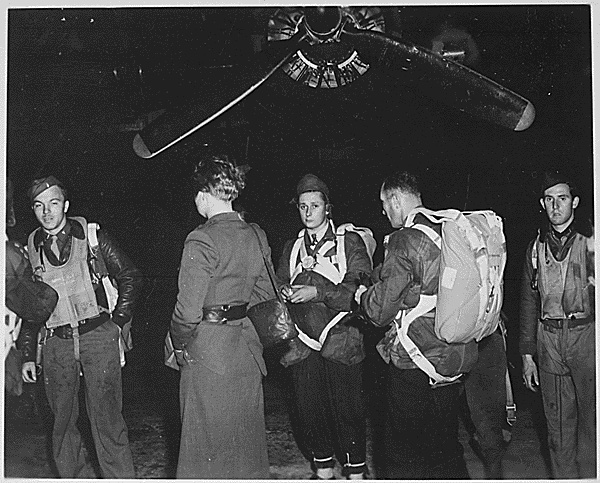
In the early 1980s, physicians and activists in Africa and Asia began sounding the alarm about an explosion of young patients dying within weeks of being infected instead of years. Hours after entering the hospital, they were choking to death on their own blood. In 1985, physicians in Zaire and Zambia noted high rates of active tuberculosis among patients who had the emerging disease now known as HIV/AIDS. TB surged globally, including in the U.S. Deaths skyrocketed. From 1985 to 2005, roughly as many people died of tuberculosis as in World War I, and many of them also had HIV. In 2000, nearly a third of the 2.3 million people who died of tuberculosis were co-infected with HIV.
By the mid-1990s, antiretroviral cocktails made HIV a treatable and survivable disease in rich communities. While a person is taking these medications, their viral levels generally become so low as to be undetectable and untransmittable; if a person with HIV becomes sick with tuberculosis, the drugs increase their odds of survival dramatically. But rich countries largely refused to spend money on HIV and TB meds in low- and middle-income countries. They cited many reasons, including that patients couldn’t be trusted to take their medication on time, and that resources would be better spent on prevention and control. In 2001, the head of the U.S. Agency for International Development had this to say when explaining to Congress why many Africans would not benefit from access to HIV medications: “People do not know what watches and clocks are. They do not use Western means for telling time. They use the sun. These drugs have to be administered during a certain sequence of time during the day and when you say take it at 10:00, people will say, ‘What do you mean by 10:00?’” A 2007 review of 58 studies on patient habits found that Africans were more likely to adhere to HIV treatment regimens than North Americans.
In the mid-2000s, programs such as PEPFAR and the Global Fund finally began distributing antiretroviral therapy to millions of people living with HIV in poor countries. PEPFAR, a U.S.-funded initiative, was especially successful, saving more than 25 million lives and preventing 7 million children from being born with HIV. These projects lowered deaths and infections while also strengthening health-care systems, allowing low-income countries to better respond to diseases as varied as malaria and diabetes. Millions of lives have been saved—and tuberculosis deaths among those living with HIV have declined dramatically in the decades since.
Still, tuberculosis is great at exploiting any advantage that humans hand it. During the COVID-19 pandemic, disruptions to supply chains and TB-prevention programs led to an uptick in infections worldwide. Last year, the U.S. logged more cases of tuberculosis than it has in any year since the CDC began keeping count in the 1950s. Two people died. But in some ways, at the beginning of this year, the fight against tuberculosis had never looked more promising. High-quality vaccine candidates were in late-stage trials. In December, the World Health Organization made its first endorsement of a TB diagnostic test, and global health workers readied to deploy it.
Now that progress is on the verge of being erased. Since Donald Trump has taken office, his administration has dismantled USAID, massively eliminating foreign-aid funding and programs. According to The New York Times, hundreds of thousands of sick patients have seen their access to medication and testing suddenly cut off. A memo released by a USAID official earlier this month estimated that cases of multidrug-resistant tuberculosis will rise by about 30 percent in the next few years, an unprecedented regression in the history of humankind’s fight against the disease. (The official was subsequently placed on administrative leave.) Research on tuberculosis tests and treatments has been terminated. Although the Secretary of State and Elon Musk have assured the public that the new administration’s actions have not disrupted the distribution of life-saving medicine, that just isn’t true. A colleague in central Africa sent me a picture of TB drugs that the U.S. has already paid for sitting unused in a warehouse because of stop-work orders. (Neither the State Department nor DOGE employees responded to requests for comment.)
Last year, roughly half of all international donor funding for tuberculosis treatment came from the U.S. Now many programs are disappearing. In a recent survey on the impact of lost funding in 31 countries, one in four organizations providing TB care reported they have shut down entirely. About half have stopped screening for new cases of tuberculosis. The average untreated case of active tuberculosis will spread the infection to 10 to 15 people a year. Without treatment, or even a diagnosis, hundreds of thousands more people will die—and each of those deaths will be needless.
By revoking money from global-health efforts, the U.S. has created the conditions for the health of people around the world to deteriorate, which will give tuberculosis even more opportunities to kill. HIV clinics in many countries have started rationing pills as drug supplies run dangerously low, raising the specter of co-infection. Like HIV, insufficient nutrition weakens the immune system. It is the leading risk factor for tuberculosis. An estimated 1 million children with severe acute malnutrition will lose access to treatment because of the USAID cuts, and refugee camps across the world are slashing already meager food rations.
For billions of people, TB is already a nightmare disease, both because the bacterium is unusually powerful and because world leaders have done a poor job of distributing cures. And yet, to the extent that one hears about TB at all in the rich world, it’s usually in the context of a looming crisis: Given enough time, a strain of tuberculosis may evolve that is resistant to all available antibiotics, a superbug that is perhaps even more aggressive and deadly than previous iterations of the disease.
The Trump administration’s current policies are making such a future more plausible. Even pausing TB treatment for a couple of weeks can give the bacterium a chance to evolve resistance. The world is ill-prepared to respond to drug-resistant TB, because we have shockingly few treatments for the world’s deadliest infectious disease. Between 1963 and 2012, scientists approved no new drugs to treat tuberculosis. Doing so stopped being profitable once the disease ceased to be a crisis in rich countries. Many strains of tuberculosis are already resistant to the 60-year-old drugs that are still the first line of treatment for nearly all TB patients. If a person is unlucky enough to have drug-resistant TB, the next step is costly testing to determine if their body can withstand harsh, alternative treatments. The United States helped pay for those tests in many countries, which means that now fewer people with drug-resistant TB are being diagnosed or treated. Instead, they are almost certainly getting sicker and spreading the infection.
Drug-resistant TB is harder to cure in individual patients, and so the aid freeze will directly lead to many deaths. But giving the bacteria so many new opportunities to develop drug resistance is also a threat to all of humanity. We now risk the emergence of TB strains that can’t be cured with our existing tools. The millennia-long history of humans’ fight against TB has seen many vicious cycles. I fear we are watching the dawn of another.
Premium IPTV Experience with line4k
Experience the ultimate entertainment with our premium IPTV service. Watch your favorite channels, movies, and sports events in stunning 4K quality. Enjoy seamless streaming with zero buffering and access to over 10,000+ channels worldwide.