In late 2024, shortly before a ceasefire curbed the violence in Gaza, I was on a monthlong medical mission to Al-Aqsa Hospital, in central Gaza, lending my emergency-medicine expertise to local doctors. Most of these doctors were displaced themselves, their homes destroyed, but they continued to show up at the emergency department as volunteers. Almost every day, we responded to a mass-casualty incident—an event that overwhelms the resources of the hospital. On many days, we experienced more than one.
On December 8th, an air strike on a tent in the Nuseirat refugee camp killed at least five people, including two parents and two children. Another air strike flattened a residential building in the Bureij refugee camp, killing at least nine. Bureij was two miles away, and we could hear the explosion from inside the hospital. We rushed to the ambulance bay, preparing to receive patients.
The first was a seven-year-old boy. Apart from very treatable entry and exit wounds behind his kneecap, he looked unscathed. At first, I thought he was lucky. Then E.M.T.s arrived cradling his baby sister Sabah, who was about six months old. Their parents had just been killed in the same attack.
I ran after Sabah into the critical-care room. Wrapped in a shiny thermal blanket, she might have looked serene if not for the tubes in her nose and mouth. I could see subtle bruising behind her eyelids. There were gaping wounds on her cheeks and fractures in her skull.
Sabah’s breathing tube had been secured in an odd way, to avoid her injuries. Medical personnel had also inserted a nasogastric tube, which normally follows intubation, to prevent vomiting. This concerned me. She probably has facial fractures, I thought. The tube could inadvertently reach her brain. Sure enough, when I looked more closely, I could see brain matter coming out of the tube. Sabah suddenly bucked. Her breathing tube came out.
I tried to guide the tube back in by placing my finger in Sabah’s tiny mouth. To my surprise, she began to suck on it. She cooed faintly. Survival instincts are buried so deep inside the central nervous system that they are unaffected even by devastating injuries. I hoped that, in whatever remained of her fragile brain, Sabah was dreaming—of her mother’s embrace, or of her father murmuring a bedtime story. An ambulance was called to take her to a CT scanner. Al-Aqsa’s CT scanner was missing a part, and it could not be replaced because of the blockade, so she would have to be driven to another hospital.
As I stood next to Sabah, my finger in her mouth, the weight of what I was experiencing overwhelmed me for the first time. I hadn’t saved her, but she hadn’t died. We were frozen somewhere in between.
When I closed my eyes, I felt tears falling. But it wasn’t sadness—I had long ago made peace with the tragedy of losing patients, even children. Instead, I was furious at the injustice around me. I wanted the world to feel what I felt. I wanted to scream and drive my fists into the walls. But I couldn’t. Whatever I was holding inside, the people around me had been carrying for at least fourteen months. I finally tore myself away from Sabah’s bed and climbed the stairs to my own.
The next morning, in a patient room that had been converted into a sleeping area, I fought wakefulness. I didn’t want to accept that the next day had arrived, because that would mean that yesterday had happened. I didn’t want to remember that, as visiting doctors, we could not leave the hospital: we could either be here, taking care of the wounded, or out there, getting wounded. A friend of mine, an emergency physician who was also from the U.S., was standing above my mattress. We were the only American doctors in the hospital that day. “I saw her CT,” she said.
Sabah had a hopeless prognosis: severe brain edema. Her brain had swollen until it was pressed against her skull. She was in the intensive-care unit, but her case was now palliative.
A day of work passed. A mass-casualty incident, then another. I tried not to think about Sabah. A sleepless night, followed by more M.C.I.s. Each wave of patients sapped what few resources we had. Strikes that were described as dismantling Hamas had killed doctors, blown up ambulances, and destroyed humanitarian infrastructure; only three of Gaza’s thirty-six hospitals were now considered operational. We knew that, even after the last bomb fell, children would continue to die—not from shrapnel but from sepsis, dehydration, and wounds that would not heal.
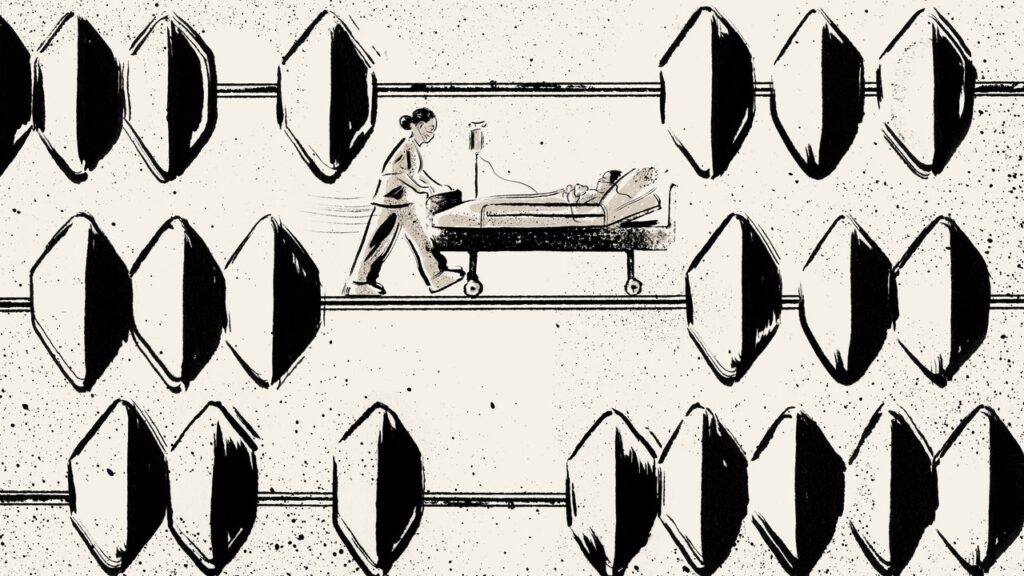
Mass-casualty incidents have a way of turning patients into numbers—not in the cruel way that news stories count bodies but more slowly, more intimately. I sometimes thought about a wooden abacus I had when I was growing up. I imagined each patient as a brightly painted bead sliding gradually across a steel rod. Sometimes, a bead caught your eye and became more than a bead. You saw its details—the grain of the wood, a chip in the paint. But the beads never stopped. The count went on.
On December 10th, I went to the I.C.U. to visit Sabah. She would be suspended between life and death until an I.C.U. doctor finally had the courage to set her ventilator to zero. I imagined her brother in the sprawl of tents outside the hospital. He had been discharged into the care of whoever had come for him that night—a neighbor, or maybe a cousin. So many parents had died that we could not wait for parents. If a child could name the person standing in front of them, they were allowed to leave.
On my way into the unit, a smiling man stopped me. He placed his hands over his chest, in the shape of a heart, and I looked quizzically at his nurse. “He was your patient in the E.R. two nights ago,” the nurse said.
Suddenly, I remembered. I had stepped away from Sabah just long enough to ultrasound him, diagnose him with pericardial tamponade—his heart was essentially drowning in blood—and start treating him. He held up seven fingers. “He went into cardiac arrest for seven minutes before his heart started again,” the nurse translated. Now he was sitting in front of me, rosy-cheeked and smiling. Only after I talked to him did the unbearable start to seem bearable. I went to Sabah’s bed and said goodbye.
In January, Israel and Hamas agreed to a ceasefire. The streets filled with zaghrouta, a trilling sound that some Arab women make at joyous occasions. People sang, danced, and cried tears of relief and joy. The first phase of the ceasefire, meant as a temporary reprieve, saw the release of twenty-five living Israeli hostages and about nineteen hundred Palestinian prisoners. Israeli forces withdrew from populated areas, allowing some displaced people to return to what was left of their neighborhoods. Still, only one border crossing was open to humanitarian aid. At the rate that it was being allowed through, the U.N. estimated, it would take three hundred and fifty years to rebuild Gaza.
As the next stage of the ceasefire approached, the agreement began to look increasingly fragile. In the face of international condemnation—but U.S. support—Israel has further restricted aid, cut electricity, and blocked medical supplies, aiming to pressure Hamas into revising the terms of the agreement and immediately releasing additional hostages. In Gaza, I saw what a collapse in the ceasefire would mean. More babies like Sabah would be born under a sky filled with buzzing military drones; more would die when bombs fell on their houses. But I also saw what could happen when a patient was given a chance.
The doctors working in the emergency department at Al-Aqsa were mostly recent medical-school graduates or general practitioners. In the previous year, they’d treated more trauma patients than many of their American counterparts would see in a decade. But they often worked without supplies, electricity, or books to learn from, and many of the senior doctors who could have offered guidance had been killed, or displaced. With no one to teach them, the physicians at Al-Aqsa often directed their resources away from patients with serious injuries—decisions that were reinforced when the patients ultimately died. In different circumstances, with proper resources and support, some of them might have survived.
Four days after Sabah came to the emergency department, there was another air strike in Nuseirat, and another child was placed on a cot in front of me. She was four years old. I was unwrapping the bandages around her head, assessing her wounds, when an emergency-medicine resident said, “Hopeless case.” The nurses around me agreed. They all said it with such certainty that I initially questioned my instincts. Someone noted that brain matter was spilling out of her head wound, which was true. But, to me, that meant an open fracture—which would leave room for the girl’s brain to decompress instead of swelling until it hit bone. “We have to try,” I told them.
As an emergency doctor, I try to analyze facts, assess risks, calculate probabilities, and create decision trees. Training develops your sense of the possible and the impossible. I felt that this girl had a chance. I Frankensteined together a vaguely child-sized artificial manual breathing unit—an Ambu bag—and connected it to a supply of oxygen. I was grateful to find a pediatric endotracheal tube.
The emergency-medicine resident, who had reached her second year in the hospital with virtually no supervision, wanted to learn how to intubate a patient. This is a fundamental skill that every emergency doctor has to know. Unless we took control of the girl’s airway, her tongue, blood, or vomit could cut off oxygen from her lungs. I made sure that the girl had one of the hospital’s few working pulse oximeters; Israel’s blockade prevented us from ordering new ones. After her oxygen level reached a hundred per cent, the nurse delivered paralyzing medication. Now the girl’s breathing was in our hands. “Ready?” I asked.
“Ready, ready,” the resident said. She started to search for the girl’s vocal cords with a laryngoscope, but she couldn’t find them. The resident’s first attempt missed—the tube was in the esophagus. (Medical supplies that could have a “dual use,” meaning that they could theoretically be repurposed in a nefarious way, are not allowed into Gaza, so we were working without a metal stylet that would normally guide the breathing tube.) I could see the resident’s frustration, the fear and anger she must have felt at being put in this situation. I could also see her determination.
After giving the girl some oxygen, the resident tried again. The girl’s paralyzing medication was wearing off; I could see her starting to gag around our instruments. We intubated her just in time to prevent her dinner—ramen noodles—from going into her lungs.
Premium IPTV Experience with line4k
Experience the ultimate entertainment with our premium IPTV service. Watch your favorite channels, movies, and sports events in stunning 4K quality. Enjoy seamless streaming with zero buffering and access to over 10,000+ channels worldwide.