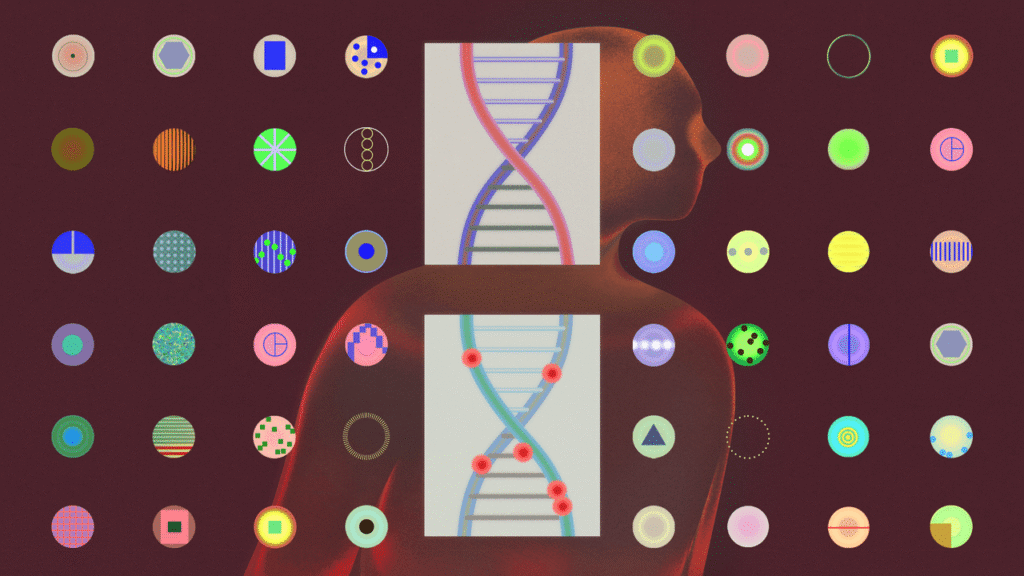
The discovery began, as many breakthroughs do, with an observation that didn’t quite make sense. In 1948, two French researchers, Paul Mandel and Pierre Métais, published a little-noticed paper in a scientific journal. Working in a laboratory in Strasbourg, they had been cataloguing the chemical contents of blood plasma—that river of life teeming with proteins, sugars, waste, nutrients, and cellular debris. Amid this familiar inventory, they’d spotted an unexpected presence: fragments of DNA drifting freely.
The finding defied biological orthodoxy. DNA was thought to remain locked inside the nuclei of cells, and not float around on its own. Stranger still, these weren’t whole genomes but broken pieces—genetic flotsam cast adrift from an unknown source.
Mandel and Métais weren’t sure what to make of it. The scientific community, equally perplexed, largely ignored the paper for more than a decade. But biological mysteries rarely remain buried. Eventually, researchers returned to the question with a simple explanation. Each day, as billions of cells perish, they rupture, spilling their contents—DNA included—into the bloodstream. These fragments circulate briefly before being metabolized or cleared by the kidneys. This “cell-free DNA,” the researchers concluded, was the residue of the body’s ongoing cycle of death and renewal.
DNA seemed to be cast off from dying cells like debris from sinking vessels. What appears as waste may serve as witness—a sock, a spoon, a necklace drifting from a submerged compartment, each hinting at a life once lived. Might these fragments in our blood carry messages from the cells that released them? Could scientists assemble these molecular scraps and reconstruct the identities of the cells they came from?
In the nineteen-sixties, Aaron Bendich, a cancer researcher in New York, proposed that tumor cells, like healthy ones, might shed DNA into the bloodstream. By 1989—four decades after Mandel and Métais’s discovery—researchers had found concrete evidence of tumor-derived cell-free DNA in cancer patients’ blood.
The implications were far-reaching. For generations, scientists had searched for ways to detect cancer early: mammograms, colonoscopies, Pap smears—all designed to catch malignancies before they spread. The idea that cancer cells might be leaking their secrets into the blood suggested a radical new possibility: that we might detect malignancy not through imaging or a physical exam but by a simple blood draw. Scientists would eventually call this a “liquid biopsy,” and, for many, it augured a transformative leap in cancer screening.
The promise of early detection—of catching cancer before it announces itself through symptoms—continues to drive research and investment in the field. But this hope may hide a more complex reality.
“If we are to beat cancer, early detection and diagnosis are arguably the most effective means we have at our disposal,” a group from Cancer Research UK declared in a 2020 commentary in The Lancet Oncology. The case for cancer screening assumes the shape of a simple narrative: a lump forms in a woman’s breast; a mammogram detects it; a biopsy confirms malignancy; a surgeon removes it before it spreads. Her life is saved.
But now imagine two women visiting a mammography clinic. Both are found to have identical-looking lumps. Both are diagnosed with early breast cancer and scheduled for surgery. Each returns home relieved, convinced that modern medicine has intervened in time. As one woman told me, recalling such a moment, “Once I knew it was inside me, I wanted it out as soon as possible. I called the surgeon’s office every hour until they gave me an appointment the next week.”
The trouble is that a mammogram reveals only the shadow of a tumor—it cannot divine the tumor’s nature. It shows the body of the cancer, not its mind: that is, a mammogram cannot tell us whether the tumor is aggressive, whether it has already spread or will remain inert. The image holds no clues to intention, to future propensities.
Suppose the first woman undergoes surgery, reassured by the idea of “early” detection, but it turns out that the cancer has sent metastatic cells beyond the reach of the scalpel. The procedure, though exacting, offers no benefit. She has endured harm without gain, the very opposite of the old medical injunction: First, do no harm.
The second woman faces the inverse. Her tumor appears ominous but is, by nature, indolent—slow-growing, noninvasive, never destined to threaten her life. Yet she, too, undergoes surgery, anesthesia, recovery. The procedure removes a tumor that posed no danger. Again: harm without benefit.
This paradox reveals a central flaw in our current model of cancer screening. We have become adept at locating cancer’s physical presence—its corporeal form—but remain largely blind to its character, its behavior, its future. We employ genomic assays and histopathological grading, but many early-stage tumors remain biologically ambiguous. They might be the kind of early cancers that surgery can cure. They might be slow-growing and unlikely to cause harm. Or, most concerning, they might already have metastasized, rendering local intervention moot. Three possibilities—yet we often cannot tell which we’re confronting.
To complicate matters further, false positives abound: tests that suggest cancer where none exists, leading to unnecessary procedures, anxiety, and harm. To begin navigating this treacherous terrain, we might turn to a curious figure—an Enlightenment-era clergyman and mathematician whose ideas now guide us through the darkness.
Thomas Bayes was no physician. Born at the start of the eighteenth century, he was a Presbyterian minister with a side gig in formal logic—an interpreter of uncertainty in an age that craved certainty. In the one portrait traditionally said to depict Bayes (though the sitter may have been misidentified), he appears as a sizable, self-assured man with a Wall Street haircut: Alec Baldwin in a clergyman’s coat. Bayes published only two papers in his lifetime: one a defense of God’s benevolence, the other a defense of Newton’s calculus. His lasting contribution came posthumously, in a Royal Society paper on conditional probability. Its argument still informs the way we assess information.
Imagine a group of a thousand heavy smokers in their sixties. One of them has lung cancer. That one-in-a-thousand chance is what Bayesians call the “prior probability”—the odds of having the disease before we know anything else. Now suppose we use a test that correctly detects lung cancer ninety-nine per cent of the time when it’s present. That’s the test’s “sensitivity.” It also correctly gives a negative result ninety-nine per cent of the time when cancer isn’t present—that’s the test’s “specificity.”
So what does it signify if someone in the group tests positive—what are the chances the person actually has cancer? Bayesian arithmetic gives a surprising answer: the test can be expected to identify the one person who actually has cancer, but it will also wrongly flag about ten people who don’t. That means there will be roughly eleven positive results, but only one of them is accurate. The chance that someone who tests positive has cancer, then, is just over nine per cent. In other words, eleven people would be sent for follow-up procedures, such as biopsies. And ten of them would go through a risky and invasive process—which can involve a punctured lung, bleeding, or other complications—with no benefit.
In short, if you set out to find a needle in a haystack, even with the best detector, you’ll mostly turn up hay. Choose a haystack with thousands of needles scattered among the bales, and you’ll start finding more needles than hay. Posterior probability (the chance that you’ve found a needle) depends on prior probability (how many needles were there to begin with).
Knowledge, in the Bayesian model, is always provisional, a process of updating one’s beliefs in light of new evidence. In a fifty-eight-year-old survivor of breast cancer with a strong family history of the disease, a new lump near the original site likely signals recurrence—intervention is warranted. In a twenty-year-old with no relevant history, the same finding is likely benign—watchful waiting may suffice.
The consequences of ignoring these principles are staggering. In 2021, according to one estimate, the United States spent more than forty billion dollars on cancer screening. On average, a year’s worth of screenings yields nine million positive results—of which 8.8 million are false. Millions endure follow-up scans, biopsies, and anxiety so that just over two hundred thousand true positives can be found, of which an even smaller fraction can be cured by local treatment, like excision. The rest is noise mistaken for signal, harm mistaken for help.
The quandaries of early detection don’t end there. I sometimes pose a question to my interns during morning rounds: “How do we judge whether a cancer-screening test is effective?” An answer usually comes quickly: “If the test detects malignancies at a high rate or at an early stage.”
But, as the mammography story illustrates, merely finding a tumor tells us nothing about what it will do. So I press further. Their next answer also comes quickly: “By dividing a population into screened and unscreened groups, then measuring which group lives longer without cancer.” But this approach invites another fallacy.
Suppose two identical twins develop breast cancer at the same time, in 2025. One undergoes regular screening; her tumor is caught early. She begins treatment—surgery, chemotherapy. The process is gruelling: a blood clot after surgery, an infection during chemo, months of recovery. Four years pass. She endures it all, hopeful for a cure.
Her sister, shaken by an old friend’s treatment ordeal, avoids screening altogether. She moves to upstate New York, tends apple trees, reads books, and shuns medical intervention. By 2029, breast-cancer symptoms appear, but she declines treatment.
In 2030, the first sister learns that her cancer has returned. She’s admitted to a hospital in New York City. That same month, her sister—now visibly ill—is admitted to the same facility. They lie in adjacent beds, reflecting on their choices. They die the same week.
Now comes the illusion. The first twin’s post-diagnosis survival is recorded as five years; the second’s, just one year. Doctors reviewing their cases might conclude that screening extended survival fivefold. But both women were born and died at the same time. The screening had no impact on life span. The apparent benefit is a statistical mirage—an artifact of when we start the clock. This is “lead-time bias,” which inflates survival time without improving outcomes.
Lead-time bias isn’t the only illusion that distorts cancer-screening results. Consider a village where a cancer occurs in two forms—one fast and fatal, the other slow and largely harmless. With annual screening, the slow-growing tumors are more likely to be flagged: they linger longer in a detectable, symptom-free phase. The aggressive ones, by contrast, often produce symptoms between screenings and are diagnosed clinically. (Patients with them can even die between annual tests.) After a decade, the data look promising: more early cancers found, longer survival after diagnosis. But the apparent benefit is misleading. Screening disproportionately detects indolent tumors—those less likely to be lethal in the first place. That’s known as length-time bias.
These twin illusions—lead-time bias and length-time bias—cast a flattering light on screening efforts. One stretches our measurement of survival by shifting the starting line; the other claims success by favoring tumors already predisposed to be less harmful. Together, they have misled cancer researchers for decades.
Premium IPTV Experience with line4k
Experience the ultimate entertainment with our premium IPTV service. Watch your favorite channels, movies, and sports events in stunning 4K quality. Enjoy seamless streaming with zero buffering and access to over 10,000+ channels worldwide.